For PBMs
Cost Containment &
Clinical Support
Services Designed Specifically for PBMs
Helping PBMs Outpace the Competition
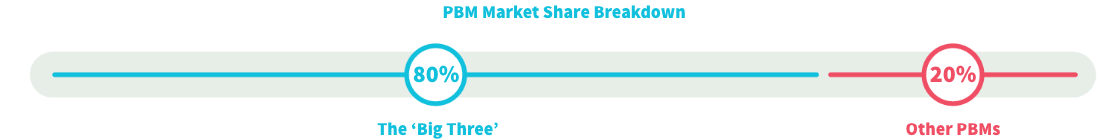
While the 'Big Three' dominate in market share, smaller PBMs lead in innovation.

ELMCRx empowers small and mid-sized PBMs with a suite of proven clinical and financial
solutions, leading to better service and savings compared to the competition.
Expand Your PBM Services
For PBMs, client success means containing pharmacy benefits costs and limiting exposure to high-cost medications, both specialty and non-specialty. Having a trusted partnership is key at every step of this process, from PBMs and TPAs to brokers, employers, and members.
Advanced Claims Technology
Considering a new claim administration solution can be a daunting and disruptive task. ELMCRx can help our partners evaluate and contract Capital Rx’s revolutionary Judi system. Whether you are a TPA or a Captive looking to upgrade your PBM program, ELMCRx can help.
Advanced Claims Technology
Considering a new claim administration solution can be a daunting and disruptive task. ELMCRx can help our partners evaluate and contract Capital Rx’s revolutionary Judi system. Whether you are a TPA or a Captive looking to upgrade your PBM program, ELMCRx can help.
Rx Clinical Management Support Soluitons
Control pharmacy costs with proven specialty and
non-specialty drug programs, including GLP-1 management, rigorous prior authorizations, and cost-effective alternatives to review and optimize pharmacy spend.
Payment Integrity & Claims Monitoring Solution
Bring contract monitoring solutions to your clients, demonstrating your commitment to transparency and compliance with fiduciary requirements.
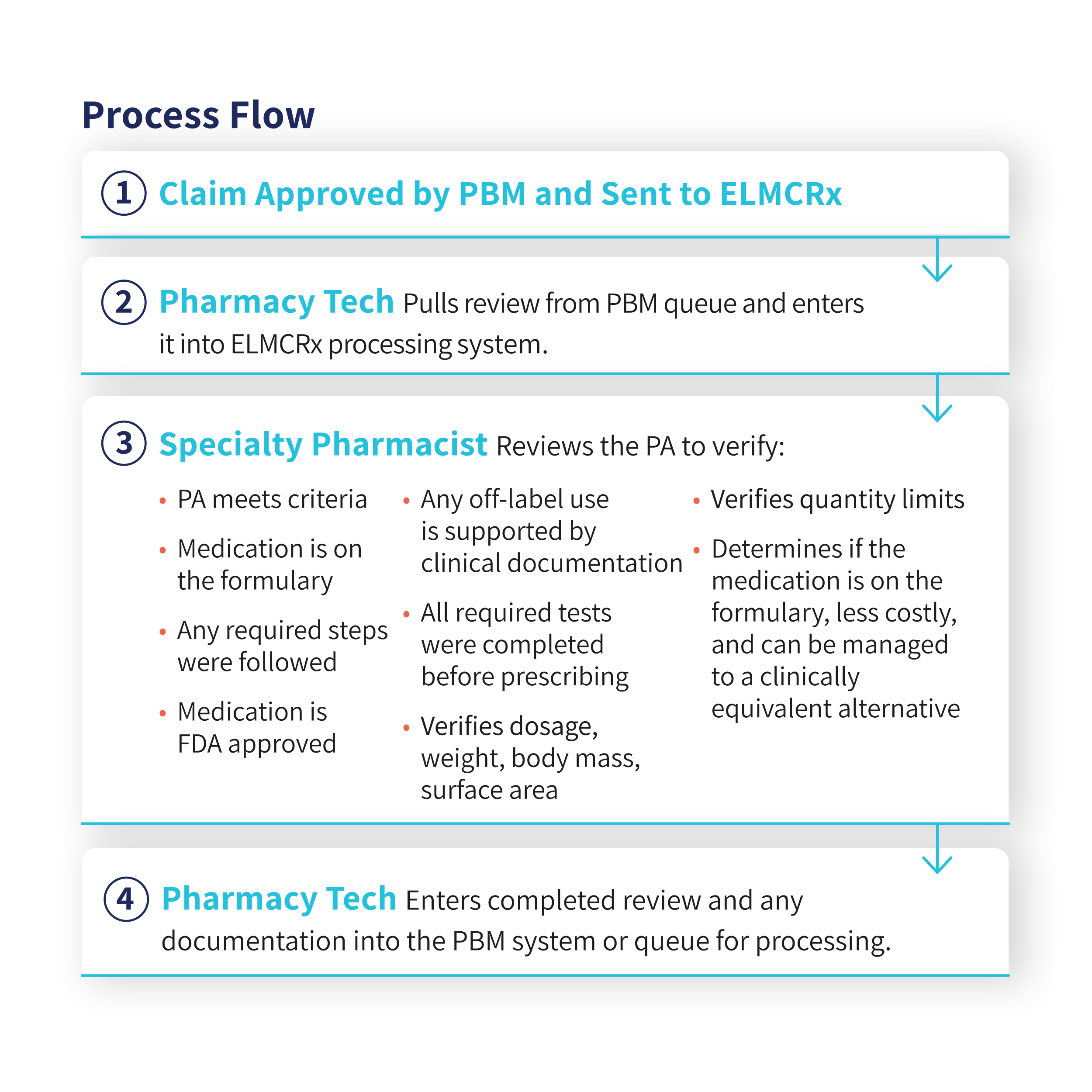
Prior Authorization Process Flow
ELMCRx has been a leader in Prior Authorization Management since 2017. As an agnostic leader
in this area, we can help you assist your clients in meeting their fiduciary requirements.
Carve Out
ELMCRx uses the PBM’s UM guidelines. Carve out by class, CEM, or other claims characteristic
Start Competing with The Big Three
Learn how ELMCRx Solutions can provide the solutions you need to expand market share and increase client savings.